What Animal Did The Rabies Start With
| Rabies | |
|---|---|
 | |
| A man with rabies, 1958 | |
| Specialty | Infectious disease |
| Symptoms | Fever, fear of water, defoliation, excessive salivary secretion, hallucinations, disrupted sleep, paralysis, coma[1] [2] Hyperactivity, Headache, Nausea, Airsickness, Feet, Vomiting.[3] |
| Causes | Rabies virus, Australian bat lyssavirus[4] |
| Prevention | Rabies vaccine, animal command, rabies immunoglobulin[one] |
| Treatment | Supportive care |
| Prognosis | Virtually 100% fatal afterwards onset of symptoms[one] |
| Deaths | 59,000 per twelvemonth worldwide[five] |
Rabies is a viral illness that causes inflammation of the brain in humans and other mammals.[1] Early symptoms can include fever and tingling at the site of exposure.[1] These symptoms are followed by one or more than of the following symptoms: nausea, vomiting, violent movements, uncontrolled excitement, fright of water, an inability to movement parts of the body, confusion, and loss of consciousness.[1] [6] [seven] [viii] One time symptoms appear, the result is almost always death, regardless of handling.[1] The time catamenia between contracting the affliction and the beginning of symptoms is usually ane to 3 months only can vary from less than one week to more than than one year.[1] The time depends on the distance the virus must travel along peripheral nerves to reach the fundamental nervous system.[ix]
Rabies is caused by lyssaviruses, including the rabies virus and Australian bat lyssavirus.[4] It is spread when an infected animal bites or scratches a human or other animals.[1] Saliva from an infected animal can also transmit rabies if the saliva comes into contact with the optics, mouth, or nose.[one] Globally, dogs are the most common animal involved.[1] In countries where dogs commonly accept the disease, more than 99% of rabies cases are the straight consequence of dog bites.[10] In the Americas, bat bites are the nigh common source of rabies infections in humans, and less than 5% of cases are from dogs.[1] [10] Rodents are very rarely infected with rabies.[x] The affliction can exist diagnosed only after the commencement of symptoms.[1]
Brute control and vaccination programs have decreased the risk of rabies from dogs in a number of regions of the earth.[1] Immunizing people before they are exposed is recommended for those at high risk, including those who work with bats or who spend prolonged periods in areas of the world where rabies is common.[1] In people who accept been exposed to rabies, the rabies vaccine and sometimes rabies immunoglobulin are constructive in preventing the disease if the person receives the handling before the first of rabies symptoms.[i] Washing bites and scratches for xv minutes with soap and h2o, povidone-iodine, or detergent may reduce the number of viral particles and may be somewhat effective at preventing transmission.[1] [11] As of 2016[update], only 14 people had survived a rabies infection after showing symptoms.[12] [13]
Rabies causes about 59,000 deaths worldwide per year,[v] about 40% of which are in children under the age of 15.[14] More than 95% of homo deaths from rabies occur in Africa and Asia.[1]
Rabies is present in more 150 countries and on all continents merely Antarctica.[ane] More than than 3 billion people alive in regions of the world where rabies occurs.[1] A number of countries, including Australia and Japan, besides every bit much of Western Europe, exercise not take rabies among dogs.[15] [sixteen] Many Pacific islands exercise not have rabies at all.[16] It is classified every bit a neglected tropical disease.[17]
Etymology
The proper name rabies is derived from the Latin rabies, "madness".[xviii] This, in turn, may be related to the Sanskrit rabhas, "to rage".[nineteen] The Greeks derived the word lyssa, from lud or "violent"; this root is used in the genus proper noun of the rabies virus, Lyssavirus.[twenty]
Signs and symptoms
Human being with rabies displaying hydrophobia

Animals with "dumb" rabies appear depressed, lethargic, and uncoordinated
The catamenia between infection and the offset symptoms (incubation menstruation) is typically one–3 months in humans.[21] This period may be as short as four days or longer than half-dozen years, depending on the location and severity of the wound and the corporeality of virus introduced.[21] Initial symptoms of rabies are often nonspecific such every bit fever and headache.[21] As rabies progresses and causes inflammation of the brain and meninges, symptoms can include slight or fractional paralysis, anxiety, insomnia, confusion, agitation, abnormal behavior, paranoia, terror, and hallucinations.[9] [21] The person may also have fright of water.[ane]
The symptoms eventually progress to delirium, and coma.[ix] [21] Expiry normally occurs 2 to x days after first symptoms. Survival is almost unknown once symptoms have presented, even with intensive care.[21] [22]
Rabies has also occasionally been referred to equally hydrophobia ("fear of h2o") throughout its history.[23] It refers to a set of symptoms in the later stages of an infection in which the person has difficulty swallowing, shows panic when presented with liquids to beverage, and cannot quench their thirst. Whatever mammal infected with the virus may demonstrate hydrophobia.[24] [ failed verification ] Saliva production is greatly increased, and attempts to drink, or even the intention or suggestion of drinking, may cause excruciatingly painful spasms of the muscles in the throat and larynx. Since the infected private cannot swallow saliva and h2o, the virus has a much higher run a risk of being transmitted, because it multiplies and accumulates in the salivary glands and is transmitted through biting.[25] Hydrophobia is commonly associated with furious rabies, which affects 80% of rabies-infected people. The remaining 20% may experience a paralytic form of rabies that is marked by musculus weakness, loss of awareness, and paralysis; this course of rabies does not ordinarily cause fearfulness of h2o.[24]
Crusade

Rendering of the rabies virus

An electron microscope paradigm of rabies virus.


Rabies is caused by a number of lyssaviruses including the rabies virus and Australian bat lyssavirus.[4] Duvenhage lyssavirus may crusade a rabies-like infection.[26]
The rabies virus is the type species of the Lyssavirus genus, in the family Rhabdoviridae, lodge Mononegavirales. Lyssavirions have helical symmetry, with a length of near 180 nm and a cross-department of about 75 nm.[27] These virions are enveloped and have a unmarried-stranded RNA genome with negative sense. The genetic data is packed every bit a ribonucleoprotein circuitous in which RNA is tightly spring by the viral nucleoprotein. The RNA genome of the virus encodes five genes whose club is highly conserved: nucleoprotein (Northward), phosphoprotein (P), matrix protein (M), glycoprotein (G), and the viral RNA polymerase (L).[28]
To enter cells, trimeric spikes on the exterior of the membrane of the virus interact with a specific jail cell receptor, the most likely one being the acetylcholine receptor. The cellular membrane pinches in a procession known equally pinocytosis and allows entry of the virus into the prison cell by way of an endosome. The virus then uses the acidic environment, which is necessary, of that endosome and binds to its membrane simultaneously, releasing its 5 proteins and single-strand RNA into the cytoplasm.[29]
Once within a muscle or nerve jail cell, the virus undergoes replication. The L protein then transcribes v mRNA strands and a positive strand of RNA all from the original negative strand RNA using gratis nucleotides in the cytoplasm. These 5 mRNA strands are then translated into their corresponding proteins (P, L, N, G and M proteins) at gratis ribosomes in the cytoplasm. Some proteins require postal service-translative modifications. For instance, the G protein travels through the rough endoplasmic reticulum, where it undergoes further folding, and is so transported to the Golgi apparatus, where a sugar grouping is added to it (glycosylation).[29]
When there are plenty viral proteins, the viral polymerase volition begin to synthesize new negative strands of RNA from the template of the positive-strand RNA. These negative strands will so course complexes with the Northward, P, L and K proteins and then travel to the inner membrane of the cell, where a One thousand protein has embedded itself in the membrane. The K poly peptide so coils around the Northward-P-L-M complex of proteins taking some of the host prison cell membrane with it, which volition grade the new outer envelope of the virus particle. The virus and then buds from the cell.[29]
From the point of entry, the virus is neurotropic, traveling forth the neural pathways into the central nervous system. The virus ordinarily outset infects musculus cells close to the site of infection, where they are able to replicate without being 'noticed' by the host'south immune organisation. Once enough virus has been replicated, they begin to bind to acetylcholine receptors at the neuromuscular junction.[xxx] The virus and so travels through the nerve cell axon via retrograde transport, every bit its P protein interacts with dynein, a poly peptide nowadays in the cytoplasm of nervus cells. Once the virus reaches the cell body it travels rapidly to the central nervous system (CNS), replicating in motor neurons and eventually reaching the brain.[9] Afterward the brain is infected, the virus travels centrifugally to the peripheral and autonomic nervous systems, eventually migrating to the salivary glands, where it is prepare to be transmitted to the side by side host.[31] : 317

Two dogs with the paralytic, or dumb, class of rabies
Transmission
All warm-blooded species, including humans, may become infected with the rabies virus and develop symptoms. Birds were first artificially infected with rabies in 1884; all the same, infected birds are largely, if non wholly, asymptomatic, and recover.[32] Other bird species take been known to develop rabies antibodies, a sign of infection, after feeding on rabies-infected mammals.[33] [34]
The virus has also adjusted to abound in cells of cold-blooded vertebrates.[35] [36] Most animals can be infected past the virus and tin can transmit the disease to humans. Worldwide, nearly 99% of human being rabies cases come from domestic dogs.[37] Other sources of rabies in humans include bats,[38] [39] monkeys, raccoons, foxes, skunks, cattle, wolves, coyotes, cats, and mongooses (normally either the small Asian mongoose or the yellow mongoose).[40]
Rabies may likewise spread through exposure to infected bears, domestic farm animals, groundhogs, weasels, and other wild carnivorans. Even so, lagomorphs, such every bit hares and rabbits, and small rodents, such as chipmunks, gerbils, guinea pigs, hamsters, mice, rats, and squirrels, are almost never found to be infected with rabies and are non known to transmit rabies to humans.[41] Bites from mice, rats, or squirrels rarely crave rabies prevention because these rodents are typically killed by any see with a larger, rabid brute, and would, therefore, not be carriers.[42] The Virginia opossum (a marsupial, unlike the other mammals named in this paragraph, which are all eutherians/placental), has a lower internal torso temperature than the rabies virus prefers and therefore is resistant only non immune to rabies.[43] Marsupials, along with monotremes (platypuses and echidnas), typically accept lower trunk tempertures than similarly-sized eutherians.[44]
The virus is usually nowadays in the fretfulness and saliva of a symptomatic rabid animal.[45] [46] The road of infection is ordinarily, just non always, by a seize with teeth. In many cases, the infected animal is exceptionally aggressive, may attack without provocation, and exhibits otherwise uncharacteristic behavior.[47] This is an example of a viral pathogen modifying the behavior of its host to facilitate its manual to other hosts. Later a typical human infection by bite, the virus enters the peripheral nervous arrangement. It and so travels retrograde along the efferent nerves toward the fundamental nervous system.[48] During this stage, the virus cannot exist easily detected within the host, and vaccination may still confer cell-mediated amnesty to forestall symptomatic rabies. When the virus reaches the brain, it speedily causes encephalitis, the prodromal phase, which is the beginning of the symptoms. Once the patient becomes symptomatic, treatment is well-nigh never constructive and mortality is over 99%. Rabies may besides inflame the spinal cord, producing transverse myelitis.[49] [l]
Although information technology is theoretically possible for rabies-infected humans to transmit it to others past biting or otherwise, no such cases have ever been documented, because infected humans are commonly hospitalized and necessary precautions taken. Casual contact, such as touching a person with rabies or contact with non-infectious fluid or tissue (urine, claret, feces), does not constitute an exposure and does not require mail service-exposure prophylaxis. But as the virus is present in sperm and vaginal secretions, it might be possible for rabies to spread through sex.[51] There are only a handful of recorded cases of human-to-human transmission of rabies, and all occurred through organ transplants from infected donors.[52] [53]
Diagnosis
Rabies can be difficult to diagnose considering, in the early stages, it is easily confused with other diseases or even with a simple aggressive temperament.[54] The reference method for diagnosing rabies is the fluorescent antibiotic test (FAT), an immunohistochemistry procedure, which is recommended past the Globe Wellness Organization (WHO).[55] The FAT relies on the ability of a detector molecule (usually fluorescein isothiocyanate) coupled with a rabies-specific antibody, forming a conjugate, to demark to and permit the visualisation of rabies antigen using fluorescent microscopy techniques. Microscopic analysis of samples is the only straight method that allows for the identification of rabies virus-specific antigen in a short time and at a reduced price, irrespective of geographical origin and status of the host. It has to be regarded as the get-go pace in diagnostic procedures for all laboratories. Autolysed samples can, all the same, reduce the sensitivity and specificity of the FAT.[56] The RT PCR assays proved to be a sensitive and specific tool for routine diagnostic purposes,[57] especially in decomposed samples[58] or archival specimens.[59] The diagnosis tin be reliably made from brain samples taken subsequently expiry. The diagnosis can likewise be fabricated from saliva, urine, and cerebrospinal fluid samples, but this is non as sensitive or reliable every bit encephalon samples.[56] Cerebral inclusion bodies called Negri bodies are 100% diagnostic for rabies infection just are found in only virtually 80% of cases.[27] If possible, the animal from which the bite was received should also be examined for rabies.[60]
Some calorie-free microscopy techniques may also be used to diagnose rabies at a tenth of the price of traditional fluorescence microscopy techniques, allowing identification of the illness in less-developed countries.[61] A exam for rabies, known equally LN34, is easier to run on a dead animal's brain and might help determine who does and does non need post-exposure prevention.[62] The exam was developed by the CDC in 2018.[62]
The differential diagnosis in a case of suspected human rabies may initially include any crusade of encephalitis, in particular infection with viruses such equally herpesviruses, enteroviruses, and arboviruses such every bit West Nile virus. The virtually important viruses to rule out are herpes simplex virus type one, varicella zoster virus, and (less commonly) enteroviruses, including coxsackieviruses, echoviruses, polioviruses, and human enteroviruses 68 to 71.[63]
New causes of viral encephalitis are also possible, equally was evidenced by the 1999 outbreak in Malaysia of 300 cases of encephalitis with a mortality rate of forty% caused past Nipah virus, a newly recognized paramyxovirus.[64] Likewise, well-known viruses may be introduced into new locales, as is illustrated by the outbreak of encephalitis due to West Nile virus in the eastern United States.[65] Epidemiologic factors, such equally season, geographic location, and the patient's age, travel history, and possible exposure to bites, rodents, and ticks, may assist directly the diagnosis.[ citation needed ]
Prevention
Almost all human exposure to rabies was fatal until a vaccine was developed in 1885 by Louis Pasteur and Émile Roux. Their original vaccine was harvested from infected rabbits, from which the virus in the nerve tissue was weakened by allowing information technology to dry for five to ten days.[66] Similar nervus tissue-derived vaccines are even so used in some countries, as they are much cheaper than mod prison cell civilisation vaccines.[67]
The human diploid cell rabies vaccine was started in 1967. Less expensive purified craven embryo cell vaccine and purified vero jail cell rabies vaccine are now available.[sixty] A recombinant vaccine called V-RG has been used in Belgium, France, Germany, and the The states to preclude outbreaks of rabies in undomesticated animals.[68] Immunization before exposure has been used in both human and nonhuman populations, where, as in many jurisdictions, domesticated animals are required to be vaccinated.[69]

A young girl about to receive PEP later existence bitten by an animal thought to be rabid
The Missouri Department of Health and Senior Services Catching Disease Surveillance 2007 Almanac Report states the following tin help reduce the take chances of contracting rabies:[70]
- Vaccinating dogs, cats, and ferrets confronting rabies
- Keeping pets under supervision
- Not handling wildlife or strays
- Contacting an animal control officer upon observing a wild animate being or a stray, specially if the animal is interim strangely
- If bitten past an brute, washing the wound with soap and h2o for 10 to xv minutes and contacting a healthcare provider to determine if postal service-exposure prophylaxis is required
28 September is Globe Rabies Day, which promotes the information, prevention, and elimination of the disease.[71]
In Asia and in parts of the Americas and Africa, dogs remain the principal host. Mandatory vaccination of animals is less constructive in rural areas. Specially in developing countries, pets may not be privately kept and their devastation may be unacceptable. Oral vaccines can be safely distributed in baits, a do that has successfully reduced rabies in rural areas of Canada, France, and the United States. In Montreal, Quebec, Canada, baits are successfully used on raccoons in the Mountain-Royal Park area. Vaccination campaigns may be expensive, merely cost-benefit analysis suggests baits may be a cost-effective method of command.[72] In Ontario, a dramatic drop in rabies was recorded when an aeriform bait-vaccination campaign was launched.[73]
The number of recorded man deaths from rabies in the United States has dropped from 100 or more than annually in the early 20th century to i or two per twelvemonth due to widespread vaccination of domestic dogs and cats and the development of homo vaccines and immunoglobulin treatments. Most deaths now issue from bat bites, which may go unnoticed by the victim and hence untreated.[74]
Handling
After exposure
Treatment subsequently exposure tin can prevent the disease if given within 10 days. The rabies vaccine is 100% effective if given early, and still has a gamble of success if delivery is delayed.[27] [29] [75] Every year, more than 15 million people go vaccinated after potential exposure. While this works well, the toll is significant.[76] In the U.s. it is recommended people receive one dose of human rabies immunoglobulin (HRIG) and 4 doses of rabies vaccine over a fourteen-day period.[77] HRIG is expensive and makes up most of the cost of postal service-exposure treatment, ranging every bit high as several grand dollars.[78] In the United kingdom of great britain and northern ireland, ane dose of HRIG costs the National Wellness Service £1,000,[79] although this is not flagged every bit a "high-cost medication".[80] A total course of vaccine costs £120–180.[81] As much as possible of HRIG should be injected around the bites, with the balance being given by deep intramuscular injection at a site distant from the vaccination site.[29]
People who have previously been vaccinated against rabies do non need to receive the immunoglobulin—only the postexposure vaccinations on days 0 and 3.[82] The side effects of modern cell-based vaccines are similar to the side effects of flu shots. The old nervus-tissue-based vaccination required multiple injections into the abdomen with a large needle but is cheap.[60] It is being phased out and replaced past affordable Earth Health Organization intradermal-vaccination regimens.[sixty] Intramuscular vaccination should be given into the deltoid, not the gluteal area, which has been associated with vaccination failure[ citation needed ] due to injection into fatty rather than musculus. In children less than a year old, the lateral thigh is recommended.[83] Thoroughly washing the wound as soon equally possible with lather and water for approximately five minutes is constructive in reducing the number of viral particles.[84] Povidone-iodine or alcohol is then recommended to reduce the virus further.[85]
Awakening to find a bat in the room, or finding a bat in the room of a previously unattended child or mentally disabled or intoxicated person, is an indication for mail service-exposure prophylaxis (PEP). The recommendation for the precautionary apply of PEP in bat encounters where no contact is recognized has been questioned in the medical literature, based on a cost–benefit analysis.[86] However, a 2002 study has supported the protocol of precautionary administration of PEP where a child or mentally compromised individual has been lone with a bat, especially in sleep areas, where a bite or exposure may occur with the victim being unaware.[87]
After onset
At least two handling schemes take been proposed for treating rabies afterwards the onset of symptoms, the Milwaukee Protocol and the Recife Protocol. The Milwaukee Protocol was first used in 2003 on Jeanna Giese, who became the first person known to accept survived rabies without preventive treatments before symptom onset. The protocol puts a person into a chemically induced coma and uses antiviral medications to prevent fatal dysautonomia. The overall protocol is circuitous; the sixth version of the protocol last updated in 2018 consists of 17 pages with 22 steps of handling, detailed monitoring, and a timeline of expected complications.[88] The Recife Protocol follows the same principle but differs in details similar termination of sedation and supplementary medication.[89]
Prognosis
Vaccination subsequently exposure, PEP, is highly successful in preventing rabies.[75] In unvaccinated humans, rabies is virtually always fatal after neurological symptoms have developed.[xc]
Epidemiology

Deaths from rabies per million persons in 2012
0
ane
2–iv
5–9
10–17
18–69
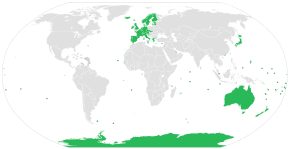
Map of rabies-complimentary countries and territories
In 2010, an estimated 26,000 people died from rabies, downwardly from 54,000 in 1990.[91] The majority of the deaths occurred in Asia and Africa.[90] As of 2015[update], India, followed by China (approximately 6,000) and the Democratic Congo-brazzaville (5,600), had the most cases.[92] A 2015 collaboration betwixt the Globe Health System, World Organisation of Fauna Health (OIE), Food and Agriculture System of the United Nation (FAO), and Global Alliance for Rabies Control has a goal of eliminating deaths from rabies past 2030.[93]
India
India has the highest rate of human being rabies in the world, primarily because of stray dogs,[94] whose number has greatly increased since a 2001 police force forbade the killing of dogs.[95] Effective control and treatment of rabies in India is hindered by a form of mass hysteria known as puppy pregnancy syndrome (PPS). Dog seize with teeth victims with PPS, male as well equally female person, go convinced that puppies are growing inside them, and often seek assistance from religion healers rather than medical services.[96] An estimated xx,000 people die every year from rabies in Republic of india, more than a 3rd of the global total.[95]
Australia
Australia has an official rabies-free status,[97] although Australian bat lyssavirus (ABLV), discovered in 1996, is a strain of rabies prevalent in Australian native bat populations. In that location have been three human cases of ABLV in Australia, all of them fatal.[ commendation needed ]
United States

Rabies cases in humans and domestic animals — Us, 1938–2018
Canine-specific rabies has been eradicated in the United States. Only rabies is common among wild animals in the United States, and an average of 100 dogs become infected from other wildlife each year.[98] [99] Bats, raccoons, skunks, and foxes business relationship for virtually all reported cases (98% in 2009). Rabid bats are constitute in all 48 contiguous states. Other reservoirs are more limited geographically; for instance, the raccoon rabies virus variant is simply found in a relatively narrow band along the East Coast.[ citation needed ]
Due to high public sensation of the virus, efforts at vaccination of domestic animals and curtailment of feral populations, and availability of postexposure prophylaxis, incidence of rabies in humans is very rare in the United states. From 1960 to 2018, a total of 125 human rabies cases were reported in the United States; 36 (28%) were attributed to canis familiaris bites during international travel.[100] Amidst the 89 infections acquired in the The states, 62 (70%) were attributed to bats.[100] The most recent rabies death in the United States was an Illinois man who refused treatment after waking up in the night with a bat on his cervix; the man died a month later on.[101] Occurring in 2021, it was the first case of human rabies in the U.s. in nearly three years.
Europe
Either no or very few cases of rabies are reported each yr in Europe; cases are contracted both during travel and in Europe.[102]
In Switzerland the affliction was virtually eliminated after scientists placed chicken heads laced with alive attenuated vaccine in the Swiss Alps.[73] The foxes of Switzerland, proven to be the main source of rabies in the country, ate the chicken heads and immunized themselves.[73] [103]
Italia, later on beingness declared rabies-free from 1997 to 2008, has witnessed a reemergence of the illness in wild animals in the Triveneto regions (Trentino-Alto Adige/Südtirol, Veneto and Friuli-Venezia Giulia), due to the spreading of an epidemic in the Balkans that also affected Austria. An all-encompassing wild animal vaccination entrada eliminated the virus from Italian republic over again, and it regained the rabies-gratis country status in 2013, the terminal reported instance of rabies being reported in a red fox in early 2011.[104] [105]
The Uk has been free of rabies since the early 20th century except for a rabies-like virus in a few Daubenton's bats. There has been one fatal instance of transmission to a human being. In that location accept been four deaths from rabies, transmitted abroad by domestic dog bites, since 2000. The last infection in the UK occurred in 1922, and the last death from indigenous rabies was in 1902.[106] [107] Different many of the other countries of Europe it is protected past being an isle, and by strict quarantine procedures.[ citation needed ]
Mexico
Mexico was certified past the Globe Wellness Organization as being free of dog-transmitted rabies in 2019 because no instance of dog-human transmission had been recorded in 2 years.[108]
History
Rabies has been known since around 2000 BC.[109] The showtime written record of rabies is in the Mesopotamian Codex of Eshnunna (circa 1930 BC), which dictates that the owner of a dog showing symptoms of rabies should take preventive measures against bites. If some other person were bitten by a rabid canis familiaris and later died, the owner was heavily fined.[110]
In Ancient Greece, rabies was supposed to be acquired past Lyssa, the spirit of mad rage.[111]
Ineffective folk remedies abounded in the medical literature of the ancient world. The md Scribonius Largus prescribed a poultice of material and hyena skin; Antaeus recommended a preparation fabricated from the skull of a hanged man.[112]
Rabies appears to accept originated in the Former World, the outset epizootic in the New World occurring in Boston in 1768.[113] It spread from at that place, over the adjacent few years, to various other states, as well as to the French West Indies, somewhen becoming common all across North America.[ commendation needed ]
Rabies was considered a scourge for its prevalence in the 19th century. In France and Belgium, where Saint Hubert was venerated, the "St Hubert's Cardinal" was heated and applied to cauterize the wound. By an awarding of magical thinking, dogs were branded with the fundamental in hopes of protecting them from rabies.
It was not uncommon for a person bitten past a domestic dog merely suspected of beingness rabid to commit suicide or to be killed past others.[20]
In aboriginal times the attachment of the natural language (the lingual frenulum, a mucous membrane) was cut and removed as this was where rabies was thought to originate. This practise ceased with the discovery of the actual cause of rabies.[31] Louis Pasteur'southward 1885 nervus tissue vaccine was successful, and was progressively improved to reduce often severe side-effects.[21]
In mod times, the fear of rabies has not diminished, and the disease and its symptoms, particularly agitation, have served equally an inspiration for several works of zombie or similarly themed fiction, often portraying rabies as having mutated into a stronger virus which fills humans with murderous rage or incurable affliction, bringing about a devastating, widespread pandemic.[114]
Other animals
Rabies is infectious to mammals; three stages of central nervous arrangement infection are recognized. The first phase is a i- to iii-day period characterized past behavioral changes and is known as the prodromal stage. The second is the excitative phase, which lasts three to iv days. This stage is often known every bit "furious rabies" for the tendency of the affected animate being to be hyper-reactive to external stimuli and bite at anything nigh. The third is the paralytic stage and is acquired by harm to motor neurons. Incoordination is seen, owing to rear limb paralysis, and drooling and difficulty swallowing is caused past paralysis of facial and pharynx muscles. Death is usually caused by respiratory abort.[116]
Research
The outer beat out of the rabies virus, stripped of its RNA contents and thus unable to cause affliction, may be used as a vector for the delivery of unrelated genetic material in a research setting. It has the advantage over other pseudotyping methods for gene delivery in that the cell targeting (tissue tropism) is more specific for the central nervous system, a difficult-to-reach site, obviating the demand for invasive delivery methods. It is likewise capable of infecting neighboring "upstream" cells, moving from one cell to axons of the next at synapses, and is thus used for retrograde tracing in neuronal circuits.[117]
Evidence indicates artificially increasing the permeability of the claret–brain barrier, which usually does not allow most allowed cells beyond, promotes viral clearance.[118] [119]
See likewise
- Global Alliance for Rabies Control
- Rabies in Haiti
- Eradication of infectious diseases
References
- ^ a b c d due east f g h i j k l thou n o p q r s t u "Rabies Fact Sheet Due north°99". World Health Organization. July 2013. Archived from the original on 1 April 2014. Retrieved 28 February 2014.
- ^ "Rabies - Symptoms and causes". Mayo Clinic . Retrieved 9 April 2018.
- ^ Dispensary, mayo clinic. "Rabies". https://world wide web.mayoclinic.org. Mayo Dispensary. Retrieved 9 June 2022.
- ^ a b c "Rabies, Australian bat lyssavirus and other lyssaviruses". The Department of Health. December 2013. Archived from the original on 4 March 2014. Retrieved 1 March 2014.
- ^ a b "Rabies". CDC. 29 July 2020. Retrieved 31 Jan 2021.
- ^ "Rabies, Symptoms, Causes, Treatment". Medical News Today. xv Nov 2017.
- ^ "Rabies, Symptoms and causes". Mayo Clinic.
- ^ "Animal bites and rabies". Johns Hopkins Medicine. 27 February 2020.
- ^ a b c d Cotran RS, Kumar V, Fausto N (2005). Robbins and Cotran Pathologic Ground of Illness (7th ed.). Elsevier/Saunders. p. 1375. ISBN978-0-7216-0187-eight.
- ^ a b c Tintinalli JE (2010). Emergency Medicine: A Comprehensive Study Guide (Emergency Medicine (Tintinalli)). McGraw-Hill. pp. Affiliate 152. ISBN978-0-07-148480-0.
- ^ Wunner WH (2010). Rabies: Scientific Basis of the Disease and Its Management. Bookish Press. p. 556. ISBN9780080550091.
- ^ Manoj S, Mukherjee A, Johri South, Kumar KV (2016). "Recovery from rabies, a universally fatal disease". Military Medical Research. 3 (1): 21. doi:10.1186/s40779-016-0089-y. PMC4947331. PMID 27429788.
- ^ Weyer, Jacqueline; Msimang-Dermaux, Veerle; Paweska, Janusz T; le Roux, Kevin; Govender, Premi; Coertse, Jessica; Markotter, Wanda; Nel, Louis H; Blumberg, Lucille H (9 June 2016). "A case of human survival of rabies, Due south Africa". Southern African Journal of Infectious Diseases. 31 (two): 66–68. doi:10.1080/23120053.2016.1128151. ISSN 2312-0053.
- ^ "Rabies: The Facts" (PDF). World Health Arrangement. Archived (PDF) from the original on 24 Feb 2017. Retrieved 24 February 2017.
- ^ WHO Expert Consultation on Rabies : second report (PDF) (2 ed.). Geneva: WHO. 2013. p. 3. ISBN9789241209823. Archived (PDF) from the original on xx Oct 2014.
- ^ a b "Rabies-Gratis Countries and Political Units". CDC. Archived from the original on 5 March 2014. Retrieved 8 May 2019.
- ^ "Neglected Tropical Diseases". cdc.gov. half-dozen June 2011. Archived from the original on four December 2014. Retrieved 28 November 2014.
- ^ Simpson DP (1979). Cassell's Latin Dictionary (5 ed.). London: Cassell. p. 883. ISBN978-0-304-52257-half dozen.
- ^ Dalfardi B, Esnaashary MH, Yarmohammadi H (Feb 2014). "Rabies in medieval Persian literature - the Catechism of Avicenna (980-1037 Ad)". Infectious Diseases of Poverty. iii (i): seven. doi:10.1186/2049-9957-3-7. PMC3933285. PMID 24533686.
- ^ a b Rotivel Y. "Introduction". Federation of American Scientists. Archived from the original on 26 April 2009. Retrieved 25 April 2009.
- ^ a b c d e f g Giesen A, Gniel D, Malerczyk C (March 2015). "xxx Years of rabies vaccination with Rabipur: a summary of clinical data and global experience". Expert Review of Vaccines (Review). fourteen (3): 351–67. doi:ten.1586/14760584.2015.1011134. PMID 25683583.
- ^ Rupprecht CE, Willoughby R, Slate D (December 2006). "Current and future trends in the prevention, treatment and control of rabies". Good Review of Anti-Infective Therapy. 4 (six): 1021–38. doi:10.1586/14787210.4.6.1021. PMID 17181418. S2CID 36979186.
- ^ Cliff AD, Haggett P, Smallman-Raynor Grand (2004). World atlas of epidemic diseases. London: Arnold. p. 51. ISBN9780340761717.
- ^ a b "Symptoms of rabies". NHS.uk. 12 June 2012. Archived from the original on 14 September 2014. Retrieved three September 2014.
- ^ "Rabies". AnimalsWeCare.com. Archived from the original on 3 September 2014.
- ^ van Thiel PP, de Bie RM, Eftimov F, Tepaske R, Zaaijer HL, van Doornum GJ, et al. (July 2009). "Fatal man rabies due to Duvenhage virus from a bat in Kenya: failure of handling with coma-induction, ketamine, and antiviral drugs". PLOS Neglected Tropical Diseases. three (7): e428. doi:x.1371/journal.pntd.0000428. PMC2710506. PMID 19636367.
- ^ a b c Drew WL (2004). "Chapter 41: Rabies". In Ryan KJ, Ray CG (eds.). Sherris Medical Microbiology (fourth ed.). McGraw Hill. pp. 597–600. ISBN978-0-8385-8529-0.
- ^ Finke S, Conzelmann KK (Baronial 2005). "Replication strategies of rabies virus". Virus Research. 111 (2): 120–31. doi:ten.1016/j.virusres.2005.04.004. PMID 15885837.
- ^ a b c d e "Rabies Post-Exposure Prophylaxis". Centers for Disease Control and Prevention (CDC). 23 Dec 2009. Archived from the original on 1 February 2010. Retrieved 30 January 2010.
- ^ Gluska S, Zahavi EE, Chein M, Gradus T, Bauer A, Finke S, Perlson E (August 2014). "Rabies Virus Hijacks and accelerates the p75NTR retrograde axonal transport machinery". PLOS Pathogens. 10 (8): e1004348. doi:10.1371/periodical.ppat.1004348. PMC4148448. PMID 25165859.
- ^ a b Baer G (1991). The Natural History of Rabies. CRC Printing. ISBN9780849367601 . Retrieved 31 October 2011.
- ^ Shannon LM, Poulton JL, Emmons RW, Woodie JD, Fowler ME (April 1988). "Serological survey for rabies antibodies in raptors from California". Periodical of Wildlife Diseases. 24 (2): 264–seven. doi:10.7589/0090-3558-24.2.264. PMID 3286906.
- ^ Gough PM, Jorgenson RD (July 1976). "Rabies antibodies in sera of wild birds". Periodical of Wildlife Diseases. 12 (3): 392–5. doi:10.7589/0090-3558-12.iii.392. PMID 16498885.
- ^ Jorgenson RD, Gough PM, Graham DL (July 1976). "Experimental rabies in a great horned owl". Journal of Wildlife Diseases. 12 (3): 444–7. doi:10.7589/0090-3558-12.3.444. PMID 16498892. S2CID 11374356.
- ^ Wong D. "Rabies". Wong's Virology. Archived from the original on iii December 2008. Retrieved 19 March 2009.
- ^ Campbell JB, Charlton K (1988). Developments in Veterinarian Virology: Rabies. Springer. p. 48. ISBN978-0-89838-390-4.
- ^ "Rabies". World Health System. 21 April 2020. Retrieved 3 May 2021.
- ^ Pawan JL (1959). "The transmission of paralytic rabies in Trinidad by the vampire bat (Desmodus rotundus murinus Wagner". Caribbean area Medical Journal. 21: 110–36. PMID 13858519.
- ^ Pawan JL (1959). "Rabies in the vampire bat of Trinidad, with special reference to the clinical form and the latency of infection". Caribbean Medical Journal. 21: 137–56. PMID 14431118.
- ^ Taylor PJ (December 1993). "A systematic and population genetic approach to the rabies problem in the yellowish mongoose (Cynictis penicillata)". The Onderstepoort Journal of Veterinarian Inquiry. 60 (iv): 379–87. PMID 7777324.
- ^ "Rabies. Other Wildlife: Terrestrial carnivores: raccoons, skunks and foxes". Centers for Affliction Control and Prevention(CDC). Archived from the original on 20 December 2010. Retrieved 23 Dec 2010.
- ^ Anderson J, Frey R (2006). "Rabies". In Fundukian LJ (ed.). Gale Encyclopedia of Medicine (3rd ed.).
- ^ McRuer DL, Jones KD (May 2009). "Behavioral and nutritional aspects of the Virginian opossum (Didelphis virginiana)". The Veterinary Clinics of North America. Exotic Animal Practice. 12 (2): 217–36, 8. doi:10.1016/j.cvex.2009.01.007. PMID 19341950.
- ^ Gaughan, John B.; Hogan, Lindsay A.; Wallage, Andrea (2015). Abstract: Thermoregulation in marsupials and monotremes, chapter of Marsupials and monotremes: nature's enigmatic mammals. ISBN9781634834872 . Retrieved xx April 2022.
- ^ The Merck Manual (11th ed.). 1983. p. 183.
- ^ The Merck manual of Medical Information (2nd Home ed.). 2003. p. 484.
- ^ Turton J (2000). "Rabies: a killer disease". National Department of Agriculture. Archived from the original on 23 September 2006.
- ^ Jackson AC, Wunner WH (2002). Rabies. Academic Press. p. 290. ISBN978-0-12-379077-iv. Archived from the original on 8 January 2014.
- ^ Lynn DJ, Newton HB, Rae-Grant Advertizing (2012). The v-Minute Neurology Consult. Lippincott Williams & Wilkins. pp. 414–. ISBN978-1-4511-0012-9.
- ^ Davis LE, King MK, Schultz JL (fifteen June 2005). Fundamentals of neurologic disease. Demos Medical Publishing. p. 73. ISBN978-1-888799-84-2. Archived from the original on 8 Jan 2014.
- ^ RabiesAlliance.org Archived 24 September 2016 at the Wayback Machine
- ^ Srinivasan A, Burton EC, Kuehnert MJ, Rupprecht C, Sutker WL, Ksiazek TG, et al. (March 2005). "Transmission of rabies virus from an organ donor to four transplant recipients". The New England Journal of Medicine. 352 (11): 1103–11. doi:10.1056/NEJMoa043018. PMID 15784663.
- ^ "Homo Rabies Prevention --- The states, 2008 Recommendations of the Advisory Commission on Immunization Practices". Centers for Disease Command and Prevention. 23 May 2008. Retrieved 11 February 2020.
- ^ Kahn CM, Line S, eds. (2010). The Merck Veterinary Manual (10th ed.). Kendallville, Indiana: Courier Kendallville, Inc. p. 1193. ISBN978-0-911910-93-three.
- ^ Dean DJ, Abelseth MK (1973). "Ch. 6: The fluorescent antibiotic test". In Kaplan MM, Koprowski H (eds.). Laboratory techniques in rabies. Monograph series. Vol. 23 (3rd ed.). World Health Organization. p. 73. ISBN9789241400237.
- ^ a b Fooks AR, Johnson N, Freuling CM, Wakeley PR, Banyard Ac, McElhinney LM, et al. (September 2009). "Emerging technologies for the detection of rabies virus: challenges and hopes in the 21st century". PLOS Neglected Tropical Diseases. iii (9): e530. doi:10.1371/periodical.pntd.0000530. PMC2745658. PMID 19787037.
- ^ Tordo Due north, Bourhy H, Sacramento D (1994). "Ch. x: PCR applied science for lyssavirus diagnosis". In Clewley JP (ed.). The Polymerase Chain Reaction (PCR) for Homo Viral Diagnosis. CRC Press. pp. 125–145. ISBN978-0-8493-4833-4.
- ^ David D, Yakobson B, Rotenberg D, Dveres Due north, Davidson I, Stram Y (June 2002). "Rabies virus detection by RT-PCR in decomposed naturally infected brains". Veterinary Microbiology. 87 (two): 111–8. doi:ten.1016/s0378-1135(02)00041-x. PMID 12034539.
- ^ Biswal M, Ratho R, Mishra B (September 2007). "Usefulness of opposite transcriptase-polymerase chain reaction for detection of rabies RNA in archival samples". Japanese Periodical of Infectious Diseases. threescore (v): 298–9. PMID 17881871.
- ^ a b c d Ly Due south, Buchy P, Heng NY, Ong S, Chhor N, Bourhy H, Vong Southward (September 2009). Carabin H (ed.). "Rabies situation in Cambodia". PLOS Neglected Tropical Diseases. three (nine): e511. doi:10.1371/journal.pntd.0000511. PMC2731168. PMID 19907631. e511.
- ^ Dürr S, Naïssengar S, Mindekem R, Diguimbye C, Niezgoda M, Kuzmin I, et al. (March 2008). Cleaveland S (ed.). "Rabies diagnosis for developing countries". PLOS Neglected Tropical Diseases. ii (3): e206. doi:10.1371/periodical.pntd.0000206. PMC2268742. PMID 18365035. e206.
- ^ a b "New Rapid Rabies Exam Could Revolutionize Testing and Handling | CDC Online Newsroom | CDC". www.cdc.gov. xvi May 2018. Retrieved 23 May 2018.
- ^ "Rabies: Differential Diagnoses & Workup". eMedicine Infectious Diseases. 3 October 2008. Archived from the original on 28 Nov 2010. Retrieved 30 Jan 2010.
- ^ Taylor DH, Straw Exist, Zimmerman JL, D'Allaire S (2006). Diseases of swine. Oxford: Blackwell. pp. 463–5. ISBN978-0-8138-1703-3 . Retrieved thirty January 2010.
- ^ Minagar A, Alexander JS (2005). Inflammatory Disorders Of The Nervous Arrangement: Pathogenesis, Immunology, and Clinical Management. Humana Press. ISBN978-1-58829-424-i.
- ^ Geison GL (April 1978). "Pasteur's work on rabies: reexamining the upstanding bug". The Hastings Centre Report. 8 (2): 26–33. doi:x.2307/3560403. JSTOR 3560403. PMID 348641.
- ^ Srivastava AK, Sardana Five, Prasad Thou, Behari G (March 2004). "Diagnostic dilemma in flaccid paralysis following anti-rabies vaccine". Neurology Republic of india. 52 (1): 132–3. PMID 15069272. Archived from the original on two August 2009.
- ^ Reece JF, Chawla SK (September 2006). "Control of rabies in Jaipur, Bharat, by the sterilisation and vaccination of neighbourhood dogs". The Veterinary Record. 159 (12): 379–83. doi:10.1136/vr.159.12.379. PMID 16980523. S2CID 5959305.
- ^ "Compendium of Brute Rabies Prevention and Control" (PDF). National Clan of Land Public Health Veterinarians. 31 Dec 2007. Archived from the original (PDF) on 12 July 2010. Retrieved 3 January 2010.
- ^ 2007 Annual Report (PDF) (Written report). Bureau of Catching Illness Command and Prevention. 2007.
- ^ "Globe Rabies 24-hour interval". Earth Health Arrangement (WHO). Archived from the original on 31 December 2011.
- ^ Meltzer MI (October–December 1996). "Assessing the costs and benefits of an oral vaccine for raccoon rabies: a possible model". Emerging Infectious Diseases. two (4): 343–ix. doi:10.3201/eid0204.960411. PMC2639934. PMID 8969251.
- ^ a b c Grambo RL (1995). The World of the Fox . Vancouver: Greystone Books. pp. 94–5. ISBN978-0-87156-377-4.
- ^ "Rabies in the U.S." Centers for Affliction Control and Prevention (CDC). 22 April 2011. Archived from the original on 31 December 2011. Retrieved 31 December 2011.
- ^ a b Lite J (8 Oct 2008). "Medical Mystery: Only One Person Has Survived Rabies without Vaccine—Simply How?". Scientific American. Archived from the original on 5 Nov 2009. Retrieved 30 Jan 2010.
- ^ "Human rabies: improve coordination and emerging technology to improve access to vaccines". World Health System. Archived from the original on 24 Feb 2017. Retrieved 23 February 2017.
- ^ "Use of a Reduced (four-Dose) Vaccine Schedule for Postexposure Prophylaxis to Preclude Human Rabies" Archived 25 July 2011 at the Wayback Automobile. Centers for Affliction Control and Prevention (CDC).
- ^ "Cost of Rabies Prevention". 11 June 2019. Archived from the original on 29 March 2016.
- ^ "BNF is but bachelor in the UK".
- ^ "Milton Keynes Formulary Formulary".
- ^ "Rabies - Vaccination". 23 October 2017.
- ^ Park'due south Textbook of Customs Medicine, 22nd edition, 2013, p 254.
- ^ "Rabies". World Health Organization. Archived from the original on xv February 2015. Retrieved ane February 2015.
- ^ "Rabies & Australian bat lyssavirus information sail". Health.vic.gov.au. Archived from the original on 18 August 2011. Retrieved 30 January 2012.
- ^ National Centre for Affliction Control (2014). "National Guidelines on Rabies Prophylaxis" (PDF). Archived from the original (PDF) on 5 September 2014. Retrieved v September 2014.
- ^ De Serres G, Skowronski DM, Mimault P, Ouakki M, Maranda-Aubut R, Duval B (June 2009). "Bats in the bedroom, bats in the belfry: reanalysis of the rationale for rabies postexposure prophylaxis". Clinical Infectious Diseases. 48 (11): 1493–1499. doi:10.1086/598998. PMID 19400689.
- ^ Despond O, Tucci M, Decaluwe H, Grégoire MC, Southward Teitelbaum J, Turgeon Northward (March 2002). "Rabies in a 9-year-old child: The myth of the seize with teeth". The Canadian Journal of Infectious Diseases. 13 (2): 121–125. doi:10.1155/2002/475909. PMC2094861. PMID 18159381.
- ^ "Milwaukee Protocol, version 6 (updated November 2018)" (PDF).
- ^ Ledesma, 50. A.; Lemos, E. R.; Horta, M. A. (2020). "Comparing clinical protocols for the treatment of human rabies: the Milwaukee protocol and the Brazilian protocol (Recife)". Revista da Sociedade Brasileira de Medicina Tropical. 53: e20200352. doi:10.1590/0037-8682-0352-2020. PMC7670764. PMID 33174958.
- ^ a b "Rabies". World Health Arrangement (WHO). September 2011. Archived from the original on 31 Dec 2011. Retrieved 31 December 2011.
- ^ Lozano R, Naghavi M, Foreman K, Lim S, Shibuya 1000, Aboyans V, et al. (Dec 2012). "Global and regional bloodshed from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Affliction Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604. S2CID 1541253.
- ^ Hampson Yard, Coudeville L, Lembo T, Sambo M, Kieffer A, Attlan M, et al. (Apr 2015). "Estimating the global brunt of endemic canine rabies". PLOS Neglected Tropical Diseases. 9 (4): e0003709. doi:10.1371/periodical.pntd.0003709. PMC4400070. PMID 25881058.
- ^ "Rabies". Globe Health System. Archived from the original on 15 February 2017. Retrieved 23 February 2017.
- ^ Dugan E (xxx April 2008). "Dead as a dodo? Why scientists fear for the future of the Asian vulture". The Independent. London. Archived from the original on 17 May 2008. Retrieved 11 October 2008.
India now has the highest rate of human rabies in the world.
- ^ a b Harris G (six August 2012). "Where Streets Are Thronged With Strays Baring Fangs". New York Times. Archived from the original on 8 August 2012. Retrieved 6 August 2012.
- ^ Medicine challenges Indian superstition | Asia | DW.DE | 31.12.2012 Archived 31 Jan 2013 at the Wayback Machine
- ^ "Essential rabies maps" Archived 17 February 2010 at the Wayback Machine. World Health Organization (WHO).
- ^ "CDC – Rabies Surveillance in the U.S.: Man Rabies – Rabies". www.cdc.gov. Archived from the original on 18 Jan 2017. Retrieved x Apr 2017.
- ^ Fox Thou (vii September 2007). "U.Southward. free of canine rabies virus". Reuters. Archived from the original on 17 May 2017. Retrieved eleven April 2017.
"We don't desire to distort that rabies has been eliminated – dog rabies virus has been," CDC rabies skilful Dr. Charles Rupprecht told Reuters in a telephone interview.
- ^ a b Pieracci EG, Pearson CM, Wallace RM, Blanton JD, Whitehouse ER, Ma 10, et al. (June 2019). "Vital Signs: Trends in Man Rabies Deaths and Exposures - United States, 1938-2018". MMWR. Morbidity and Bloodshed Weekly Report. 68 (23): 524–528. doi:x.15585/mmwr.mm6823e1. PMC6613553. PMID 31194721.
- ^ "A Homo Died From Rabies In Illinois. Here'south Why That's So Unusual In The U.S." NPR. 29 September 2021.
- ^ "SURVEILLANCE REPORT - Almanac Epidemiological Report for 2015 - Rabies, ECDC (European Centre for Disease Prevention and Control)" (PDF) . Retrieved 30 August 2018.
- ^ "Switzerland ended rabies epidemic by air dropping vaccinated chicken heads from helicopters / thefactsource.com". 20 November 2019. Retrieved 10 December 2019.
- ^ "Rabies in Africa: The RESOLAB network". 29 June 2015. Archived from the original on three August 2016. Retrieved 18 April 2016.
- ^ "Ministero della Salute: "Italia è indenne dalla rabbia". l'Ultimo caso nel 2011 - Quotidiano Sanità". Archived from the original on iii June 2016. Retrieved xviii April 2016.
- ^ "Rabies". NHS. 23 February 2017. Retrieved thirty August 2018.
- ^ "Q&A: Rabies". BBC News. 17 April 2015. Retrieved 30 August 2018.
- ^ "Cómo México se convirtió en el primer país del mundo libre de rabia transmitida por perros". BBC News. 12 November 2019. Retrieved 12 Nov 2019.
- ^ Adamson PB (1977). "The spread of rabies into Europe and the likely origin of this illness in antiquity". Journal of the Royal Asiatic Society of Bang-up Uk & Republic of ireland. Imperial Asiatic Society of Great Britain and Ireland. 109 (2): 140–4. doi:10.1017/S0035869X00133829. JSTOR 25210880. PMID 11632333.
- ^ Dunlop RH, Williams DJ (1996). Veterinary Medicine: An Illustrated History. Mosby. ISBN978-0-8016-3209-9.
- ^ "Rabies: an ancient illness".
- ^ Barrett Advertisement, Stanberry LR (2009). Vaccines for Biodefense and Emerging and Neglected Diseases. Bookish Press. p. 612. ISBN9780080919027. Archived from the original on 28 April 2016. Retrieved 8 January 2016.
- ^ The Natural History of Rabies Archived two March 2016 at the Wayback Machine
The first major epizootic in North America was reported in 1768, continuing until 1771 when foxes and dogs carried the disease to swine and domestic animals. The malady was and then unusual that information technology was reported as a new disease - ^ Than K (27 October 2010). "'Zombie Virus' Possible via Rabies-Flu Hybrid?". National Geographic. Archived from the original on thirteen September 2015. Retrieved 13 September 2015.
- ^ Santo Tomás Pérez, Magdalena (2002). La asistencia a los enfermos en Castilla en la Baja Edad Media. Universidad de Valladolid. pp. 172–173. ISBN84-688-3906-X – via Biblioteca Virtual Miguel de Cervantes.
- ^ Ettinger SJ, Feldman EC (1995). Textbook of Veterinary Internal Medicine (4th ed.). W.B. Saunders Company. ISBN978-0-7216-6795-9.
- ^ Carpentier DC, Vevis K, Trabalza A, Georgiadis C, Ellison SM, Asfahani RI, Mazarakis ND (July 2012). "Enhanced pseudotyping efficiency of HIV-one lentiviral vectors by a rabies/vesicular stomatitis virus chimeric envelope glycoprotein". Factor Therapy. 19 (7): 761–74. doi:x.1038/gt.2011.124. PMID 21900965.
- ^ Roy A, Hooper DC (August 2007). "Lethal silver-haired bat rabies virus infection can exist prevented by opening the blood-brain barrier". Periodical of Virology. 81 (xv): 7993–8. doi:10.1128/JVI.00710-07. PMC1951307. PMID 17507463.
- ^ Roy A, Phares TW, Koprowski H, Hooper DC (Feb 2007). "Failure to open up the blood-brain bulwark and deliver immune effectors to fundamental nervous system tissues leads to the lethal consequence of silver-haired bat rabies virus infection". Periodical of Virology. 81 (3): 1110–8. doi:10.1128/JVI.01964-06. PMC1797506. PMID 17108029.
External links
| | Wikimedia Commons has media related to Rabies. |
| | Look up rabies in Wiktionary, the costless dictionary. |
- Rabies at Curlie
- "Rabies". Centers for Disease Control and Prevention. Retrieved 12 August 2012.
- Virus Pathogen Database and Assay Resource (ViPR): Rhabdoviridae
- OIE's Rabies Portal Archived thirteen August 2020 at the Wayback Machine
- Aerophobia and Hydrophobia in Rabies Videos
- "Rabies virus". NCBI Taxonomy Browser. 11292.
Source: https://en.wikipedia.org/wiki/Rabies#:~:text=Almost%20all%20human%20exposure%20to,for%20five%20to%20ten%20days.
Posted by: vitelafaidn1989.blogspot.com

0 Response to "What Animal Did The Rabies Start With"
Post a Comment